CRISPR gene editing is revolutionizing the landscape of medical science, particularly in the quest for solutions to devastating genetic diseases like sickle cell anemia. This powerful technology allows researchers to make precise modifications to the DNA of living organisms, bringing hopes of cures closer to reality. However, the ethical implications of gene editing provoke intense debate among scientists, ethicists, and healthcare advocates. Questions about health equity arise when discussing the potential costs of treatments—such as the sickle cell cure, which carries a hefty price tag—highlighting the disparities that could emerge in access to this groundbreaking technology. As we stand on the brink of a new era in genetic modification, society must wrestle with the responsibility that comes with CRISPR technology and its profound impact on human health.
The advent of CRISPR gene editing, often referred to as CRISPR-Cas9, marks a transformative moment in genetic research, promising to redefine our approach to treating hereditary conditions. This gene-altering method, which allows scientists to intricately select and edit specific DNA sequences, raises pertinent questions about the broader implications of genetic alterations. Alternative phrases such as ‘genetic repair technologies’ and ‘DNA modification tools’ are often used interchangeably when discussing the potential of CRISPR. With the ability to address ailments like sickle cell, the need for discourse surrounding the ethical ramifications of such advancements becomes increasingly crucial. Furthermore, the dialogue around health equity in the context of these innovations emphasizes the necessity for fair access, ensuring that the benefits of genetic breakthroughs are not limited to a select few.
Understanding CRISPR Gene Editing Innovations
CRISPR gene editing has transformed the landscape of genetic research and therapeutic interventions. This revolutionary technology allows scientists to make precise changes to DNA, enabling the potential for curing genetic disorders like sickle cell disease. By editing the genes responsible for such conditions, researchers are hopeful about providing long-term relief and enhancing the quality of life for those affected. The ability to manipulate individual genes, as seen with CRISPR, raises questions about the future of treatments for various genetic conditions. The implications of this technology are profound, not only for medicine but also for ethical discussions surrounding genetic modification.
Moreover, the advent of CRISPR technology opens new avenues for research into more complex genetic interactions. However, with these advancements come significant ethical considerations, particularly regarding the potential misuse of genetic manipulation. Applying CRISPR gene editing could lead to unintended consequences, such as altering traits that may not necessarily be harmful or enhancing attributes considered beneficial. This underscores the importance of establishing guidelines and regulatory frameworks governing gene editing practices, ensuring that we proceed cautiously in this new frontier of genetic modification.
Ethical Implications of Gene Editing Advances
The ethical implications surrounding CRISPR gene editing cannot be understated. As we delve into the capabilities of this technology, it prompts a critical examination of the choices we make regarding the human genome. The discussion around whether to eliminate genetic disorders such as sickle cell disease confronts deeper moral questions. Are we justified in ‘playing God’? What are the responsibilities that come with the power to edit the human genome? Such dilemmas are central to conversations about health equity, particularly when considering who can afford the treatment and who may be left behind.
In recent discussions, experts like Neal Baer highlight the cautionary tales associated with manipulating the human genome. They question the societal implications of selecting traits, such as in the case of potentially altering a child’s sensory capabilities based on parental preferences. This raises the concern of potential eugenics—a situation where certain traits are favored over others, fostering a society that values conformity over diversity. As we navigate these ethical waters, it is crucial to prioritize fairness and justice in health outcomes across different populations, ensuring all individuals have equitable access to the benefits of gene editing.
Sickle Cell Cure: Hope and Health Equity
The pursuit of a sickle cell cure through CRISPR gene editing represents a beacon of hope for many individuals affected by this painful condition. With the ability to edit somatic cells, researchers have made significant advancements, showing that it’s possible to eliminate the defective genes responsible for sickle cell disease. The excitement surrounding these breakthroughs is palpable, as patients may no longer have to endure the relentless complications associated with their illness. However, this promise of a cure is not without its challenges, particularly regarding access to such advanced therapeutic options.
Health equity emerges as a critical concern in the context of CRISPR technology and sickle cell treatment. The exorbitant cost of gene editing therapies—estimated at around $2.2 million—raises significant barriers for many families struggling with sickle cell disease. This brings into question who will have access to these life-altering treatments and highlights disparities in healthcare that persist across different socioeconomic and racial groups. To fully realize the benefits of scientific progress, it is essential to address these disparities and work towards health justice, ensuring that all individuals, regardless of their background, can access the latest innovations in gene editing.
The Role of Bioethics in Genetic Modification
As CRISPR technology advances, the role of bioethics becomes increasingly pivotal in shaping guidelines and regulations related to gene editing. Discussions led by experts in the field, such as Rebecca Weintraub Brendel, emphasize the need for a robust ethical framework to guide the use of gene editing in medicine. With the powerful capabilities of CRISPR, ethical considerations must weigh heavily on decisions regarding which genetic traits to modify or eliminate. The integration of bioethics into genetic research helps navigate complex questions about identity, disability, and the societal implications of enhancement versus treatment.
Moreover, bioethics promotes a dialogue about the moral responsibilities accompanying scientific innovations. Stakeholders in the healthcare community, including researchers, clinicians, and policymakers, are urged to collaborate in establishing protocols that prioritize patient welfare and societal values. The goal is not merely to advance scientific knowledge but to ensure that such advancements are tempered by ethical considerations. This commitment to ethical oversight represents a vital step in fostering public trust in gene editing technologies and ensuring that these innovations serve the well-being of all.
Genetic Editing: A Double-Edged Sword
While CRISPR gene editing offers transformative potential in addressing genetic disorders, it is also a double-edged sword. The ability to manipulate genes carries risks, including unintended and unknown consequences that may arise from such interventions. Scientists like Baer caution against an overly enthusiastic embrace of gene editing without thorough investigation into its long-term effects on human genetics. For instance, modifying genes linked to conditions like high cholesterol can have intricate implications that extend beyond the intended outcome, highlighting the intricate nature of genetic interactions.
Furthermore, the prospect of genetic editing invites visions of ‘designer babies’, where attributes such as intelligence, beauty, or athleticism can be artificially selected. This raises ethical questions about the type of society we wish to build and the criteria by which we measure ‘success’ or ‘desirability’. As we continue to explore the capabilities of CRISPR, ongoing dialogue must address not only the technical feasibility but the societal values and ethical frameworks that should guide its application. The conversation must continually balance innovation with caution, ensuring the responsible use of genetic technology.
Access to CRISPR Technologies: A Global Perspective
The global landscape of access to CRISPR technologies reveals significant disparities that underscore the need for an equitable approach to genetic editing developments. While countries like the United States are at the forefront of gene editing research, many regions around the world lack the resources necessary to participate in or benefit from these advancements. This disparity raises critical questions about who will have access to life-saving treatments and who may be excluded from the benefits of CRISPR due to socioeconomic factors.
Furthermore, as gene editing technology evolves, it is critical to establish international standards that ensure equitable access. Policies must be developed that facilitate collaboration and knowledge-sharing between countries, allowing underrepresented populations to benefit from scientific advancements. Global health equity becomes a key focus as we ponder how to distribute the benefits of CRISPR technology fairly, ensuring that innovations do not exacerbate existing health disparities but instead bridge the gap towards better healthcare for all.
Potential Consequences of Gene Editing
Gene editing, while promising, is fraught with potential consequences that require careful evaluation. Baer’s discussion about unintended effects emphasizes the complexities of genetic interactions that could arise from CRISPR applications. A seemingly straightforward modification may have ripple effects within an individual’s genome, impacting multiple biological systems in ways that scientists may not yet fully understand. This unpredictability necessitates rigorous research and monitoring to assess the long-term impacts of gene editing on human health.
Moreover, concerns about the ethical use of CRISPR extend beyond the immediate medical applications to broader societal ramifications. As debates about editing genes for enhancement purposes intensify, it becomes crucial to consider whose voices are being heard in these conversations. Are we accounting for the perspectives of those who are directly affected, such as individuals with disabilities or chronic conditions? Ensuring that diverse viewpoints are included in discussions surrounding the future of genetic modification is essential for promoting a comprehensive understanding of its implications.
The Future of Genetic Engineering and Public Perception
As CRISPR technology continues to advance, public perception will play a significant role in its acceptance and integration into healthcare practices. Awareness and understanding of gene editing’s potential and risks are pivotal in shaping the narrative surrounding its use. Scientists, policymakers, and healthcare professionals must engage with the community to foster informed discussions that demystify the science behind genetic engineering, addressing fears while clarifying the benefits.
Public engagement can also aid in establishing trust between researchers and the communities they serve. For genetic editing to be embraced widely, there must be transparency and accountability in how CRISPR is applied in clinical settings. Additionally, understanding the ethical implications and health justice considerations tied to gene editing remains crucial in building a collective vision for a future where technology serves humanity equitably. As we navigate this complex landscape, the collaborative efforts of all stakeholders will be vital in shaping a positive trajectory for genetic engineering.
Health Justice and the Inaccessibility of Advanced Treatments
The issue of health justice looms large in discussions about CRISPR gene editing and its associated costs. The staggering price tag of treatments, like the sickle cell cure, raises profound questions about accessibility and who ultimately benefits from breakthrough medical innovations. For many families, the financial burden may render life-saving gene therapies unattainable, thereby accentuating existing health disparities within marginalized communities. This scenario highlights the ethical imperative to address inequities in healthcare access and ensure that all individuals can share in the promise of genetic advancements.
Moreover, as we tread into the realm of CRISPR, it is essential to advocate for policies that promote fair pricing and equitable healthcare delivery systems. Discussions surrounding healthcare reform must encompass the implications of gene editing technologies and how they can be harnessed to improve outcomes for underrepresented populations. A commitment to health equity, coupled with a focus on justice, allows society to envision a future where innovative genetic treatments are available to everyone, irrespective of their economic situation. Balancing the scales of justice is not only a moral obligation but also crucial for fostering a healthier global population.
Frequently Asked Questions
What is CRISPR gene editing and how does it relate to the sickle cell cure?
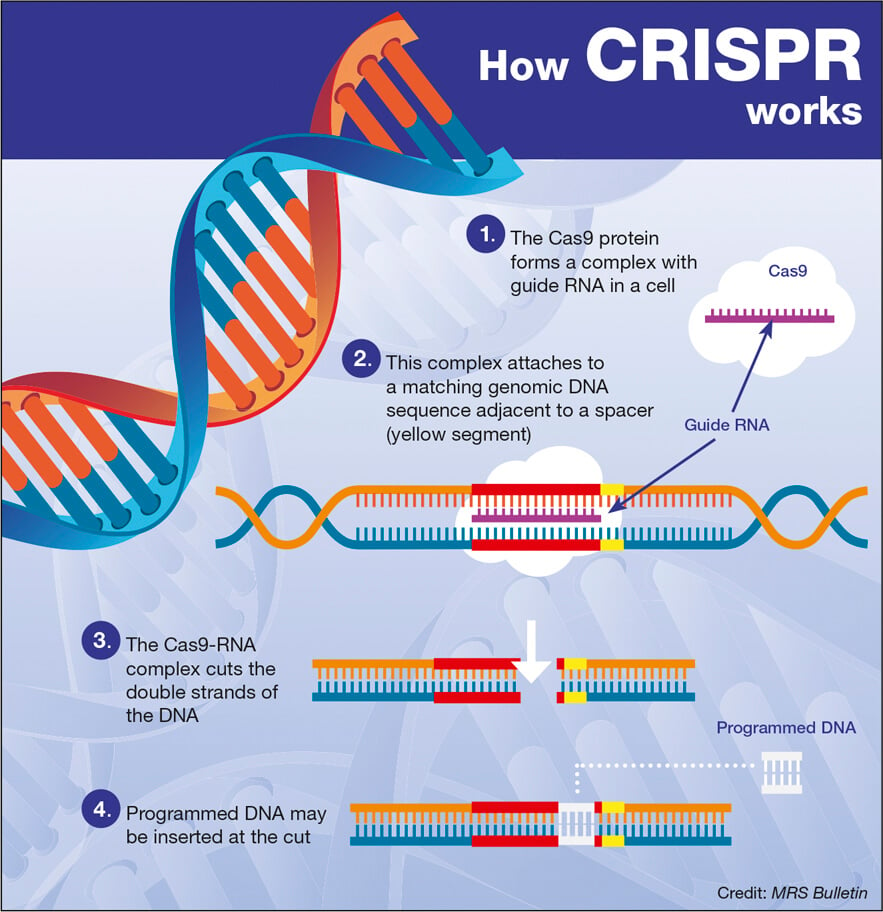
CRISPR gene editing is a revolutionary technology that allows scientists to precisely modify an organism’s DNA. It can edit both somatic and germline genes, meaning it can alter existing cells or change the genetic makeup at the embryonic level. In the case of sickle cell disease, CRISPR technology enables the correction of the faulty genes responsible for this condition, potentially providing a permanent cure for affected individuals.
What are the ethical implications of gene editing with CRISPR technology?
The ethical implications of gene editing through CRISPR technology are significant and complex. They include concerns about who decides which traits to modify, the potential for ‘designer babies’, and the broader impacts on society and health equity. For instance, should CRISPR be used only for severe genetic disorders, or also for conditions like Down syndrome, which are compatible with life? These questions challenge existing beliefs about genetics and personal choice.
How does CRISPR gene editing raise concerns about health equity?
CRISPR gene editing raises health equity concerns primarily due to the costs associated with these therapies. For example, the treatment for sickle cell disease using CRISPR can exceed $2 million per patient. This raises questions about who can afford such treatments and whether only wealthy individuals will benefit from advancements in CRISPR technology, potentially widening the gap between different socio-economic groups.
Can CRISPR technology lead to unintended consequences in genetic modification?
Yes, while CRISPR technology shows great promise in genetic modification, it can also lead to unintended consequences. Alterations made to one gene can inadvertently affect others, given that genes interact in complex ways. For instance, a recent CRISPR breakthrough aimed at lowering LDL cholesterol has highlighted that such interventions could interfere with critical biological processes, leading to unforeseen health issues.
What role does oversight play in the application of CRISPR gene editing?
Oversight is crucial in the application of CRISPR gene editing to ensure ethical standards are met and safety is maintained. Currently, while some regulations exist against practices like germline editing, there are concerns about enforcement and monitoring, particularly in countries where such regulations might be more lax. A comprehensive regulatory framework is necessary to prevent misuse and ensure that gene editing technologies are applied responsibly.
What questions arise regarding parental decisions in CRISPR gene editing?
The use of CRISPR gene editing raises deep questions about parental decisions regarding genetic modifications for their children. For instance, if parents who are deaf choose to edit their child’s genes for hearing, or if parents consider editing traits they perceive as undesirable, it begs the question: should parents have the authority to make such changes? This debate highlights the intersections of ethics, parental rights, and the definition of normalcy in human traits.
| Key Points | Details |
|---|---|
| Promise of CRISPR | CRISPR holds potential to cure genetic disorders such as sickle cell anemia. |
| Ethical Dilemmas | Questions arise about altering human traits, particularly in cases like Down syndrome. |
| Cost of Treatment | The cost of CRISPR treatments can be exorbitant, impacting access and equality. |
| Health Justice | New innovations may widen health disparities without ethical considerations. |
| Unintended Consequences | Editing one gene could affect many others, complicating outcomes. |
| Need for Oversight | There are concerns over the lack of regulation in gene editing globally. |
Summary
CRISPR gene editing represents a significant breakthrough in medical science, offering the potential to address genetic disorders like sickle cell anemia. However, with such advancements come complex ethical dilemmas about the appropriate limits of genetic modification, including the implications of altering traits considered normal variations among humans. The conversation surrounding CRISPR not only highlights the innovative capabilities of this technology but also emphasizes the critical need for responsible governance to ensure health equity and justice in access to these groundbreaking therapies.